In April 2016, China reported the last case of local primary malaria. More than five years later, the World Health Organization (WHO) announced that China had passed the malaria elimination certification. However, on a global scale, the burden of malaria is still serious, especially in Africa, the hardest-hit area, where more than 90% of global malaria cases are in Africa each year.
Professor Patrick Duffy, director of the Malaria Immunization and Vaccinology Laboratory of the National Institute of Allergy and Infectious Diseases, and others believe that when the global burden of malaria has stagnated, it has a lasting effect. The development of a vaccine for immunity is imminent.  On the evening of June 30, Beijing time, top academic The journal Nature published an online paper by Duffy and colleagues titled “Two chemoattenuated PfSPZ malaria vaccines induce sterile hepatic immunity”, reporting a malaria vaccine strategy: inoculating weakened malaria parasites and then using preventive Drug therapy showed a high level of protection in a trial involving 56 subjects.
On the evening of June 30, Beijing time, top academic The journal Nature published an online paper by Duffy and colleagues titled “Two chemoattenuated PfSPZ malaria vaccines induce sterile hepatic immunity”, reporting a malaria vaccine strategy: inoculating weakened malaria parasites and then using preventive Drug therapy showed a high level of protection in a trial involving 56 subjects.
“Nature” also published a commentary on the opinions of Nana K. Minkah and others from the Global Infectious Disease Research Center of Seattle Children’s Research Institute at the same time. Minkah et al. commented that Duffy et al. reported a vaccination strategy using live, complete Plasmodium falciparum, which provides a high level of protection against infection. “This work was achieved in the search for an effective malaria vaccine. Major progress.”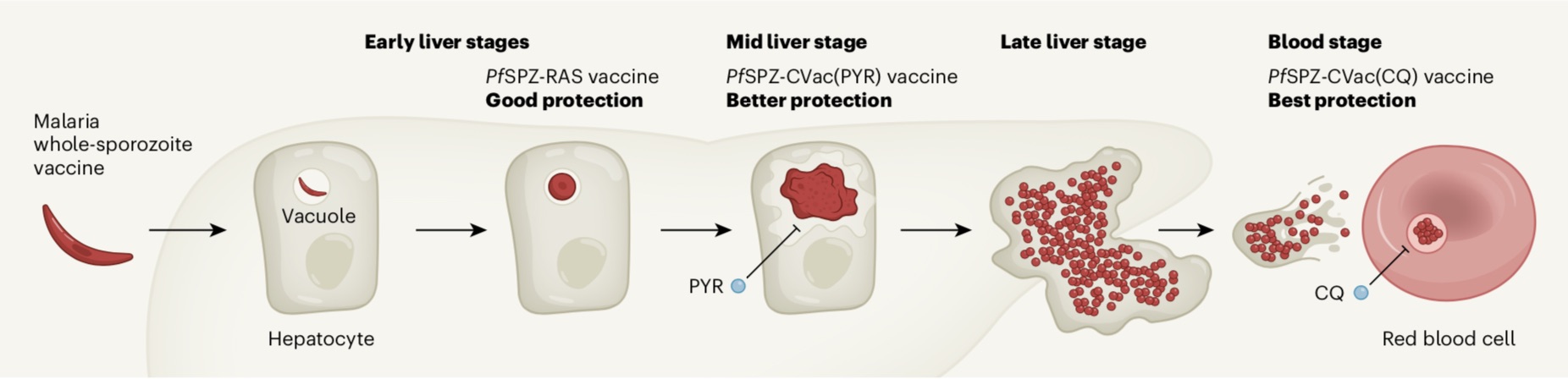 Malaria is caused by Plasmodium falciparum (Plasmodium falciparum) caused by this parasite and spread by the bite of an infected mosquito. In the human body, spore-like parasites are called sporozoites, which enter the liver and replicate in liver cells. Thousands of infectious parasites are then released into the bloodstream, infecting red blood cells. The first stage of human infection occurs in the liver, and no symptoms of disease appear in the liver stage. The second stage occurs in the blood, but it can cause disease or even death in the blood stage.
Malaria is caused by Plasmodium falciparum (Plasmodium falciparum) caused by this parasite and spread by the bite of an infected mosquito. In the human body, spore-like parasites are called sporozoites, which enter the liver and replicate in liver cells. Thousands of infectious parasites are then released into the bloodstream, infecting red blood cells. The first stage of human infection occurs in the liver, and no symptoms of disease appear in the liver stage. The second stage occurs in the blood, but it can cause disease or even death in the blood stage.
Although 140 years ago,Scientists have determined that the malaria parasite is the pathogen of malaria, but so far there has not yet been a vaccine that provides a high level of protection against malaria parasite infections on the market. Plasmodium has about 5,300 genes. The complexity of its genome and the complicated life cycle of the parasite hinder the development of vaccines.
Sporangia and the hepatic stage are called the PE stage, and have been the target of malaria vaccine development since more than 50 years ago. Duffy et al. briefly reviewed the history of malaria vaccine development in the paper. In the 1980s, GlaxoSmithKline (GSK) began to develop the malaria vaccine candidate RTS.S (trade name Moquirix), which targets a major surface protein of Plasmodium falciparum spores, the cyclosporidium protein CSP. Clinical trials show that the vaccine can prevent about 40% of malaria cases, including about 30% of life-threatening severe malaria.
However, considering the limitations of the single-protein vaccine method, vaccines using live PE parasites that infect the liver but do not cause malaria have gradually received greater attention. Immunization with replication-deficient Plasmodium falciparum radiation-attenuated sporozoites (PfSPZ-RAS) is the most studied pan-parasite vaccine so far. The candidate vaccine Sanaria PfSPZ has a protective effect on both homologous (ie the same P. falciparum strain in the vaccine) and heterologous (different strains) CHMI (Controlled Human Malaria Infection) situation and the natural transmission environment in Africa.
In this latest study, Duffy and his colleagues optimized the chemopreventive vaccination (CVac) regimen, which is based on pyrimethamine (PYR) or chloroquine (CQ Under the preventive nature of ), inoculation with sterile, purified, cryopreserved, infectious Plasmodium falciparum sporozoites (PfSPZ), pyrimethamine and chloroquine can kill parasites in the hepatic and blood stages, respectively.
The research team provided immunizations to 56 healthy adult volunteers, and a few days later, provided the volunteers with a dose of pyrimethamine or chloroquine. They evaluated the efficacy of the vaccine against both homologous and heterologous controlled human malaria infections (CHMI) after 3 months of immunization.
Studies have found that higher doses of vaccines are related to higher levels of vaccine efficacy. After the dose of PfSPZ-CVac (PYR) was increased by 4 times, the protective efficacy of the vaccine against homologous CHMI increased from 22.2% to 87.5; at high doses, the protective efficacy of the vaccine against heterologous CHMI was 77.8%. 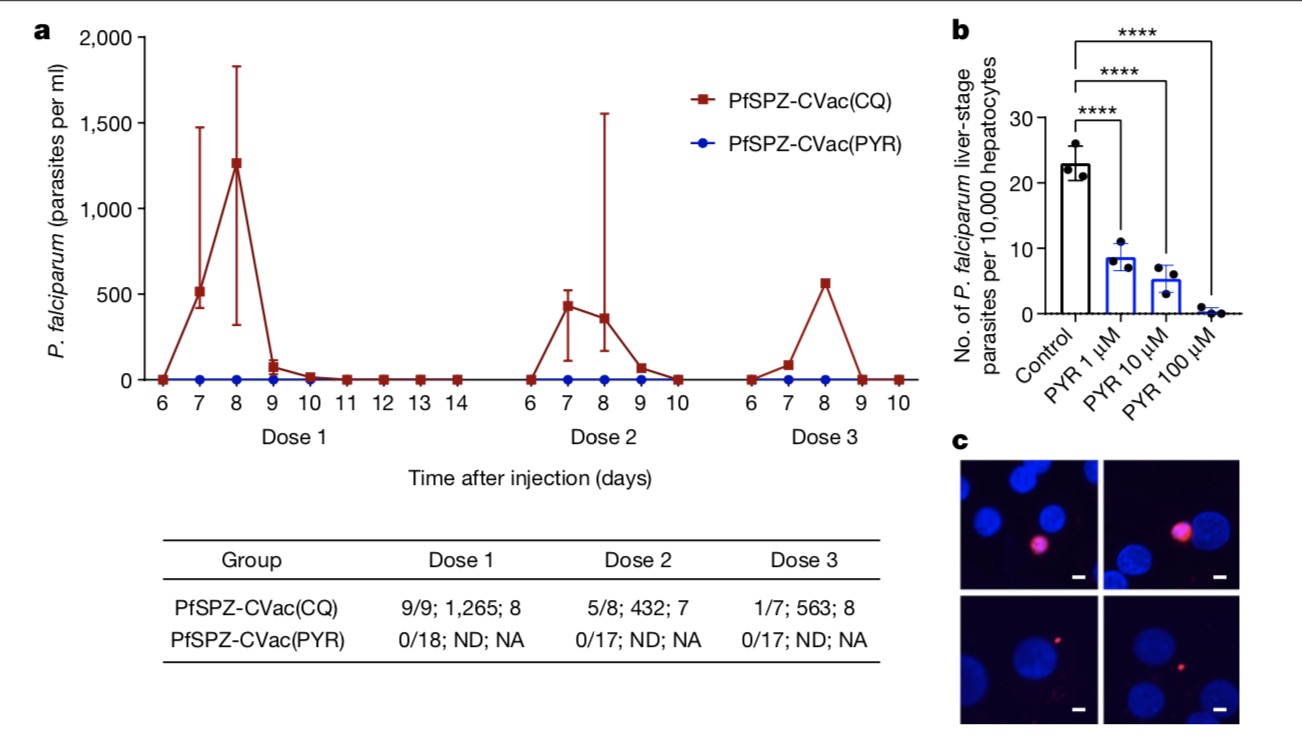 The PfSPZ-CVac(CQ) program is even better. It uses high-dose chloroquine and simultaneously immunizes with infectious spores. It targets the 7G8 strain found in Brazil and achieves it in 6 people. 100% protection effect for up to three months. This verifies the important non-specific protection effect, because an effective vaccine must have protection against various natural circulating strains of Plasmodium falciparum.
The PfSPZ-CVac(CQ) program is even better. It uses high-dose chloroquine and simultaneously immunizes with infectious spores. It targets the 7G8 strain found in Brazil and achieves it in 6 people. 100% protection effect for up to three months. This verifies the important non-specific protection effect, because an effective vaccine must have protection against various natural circulating strains of Plasmodium falciparum.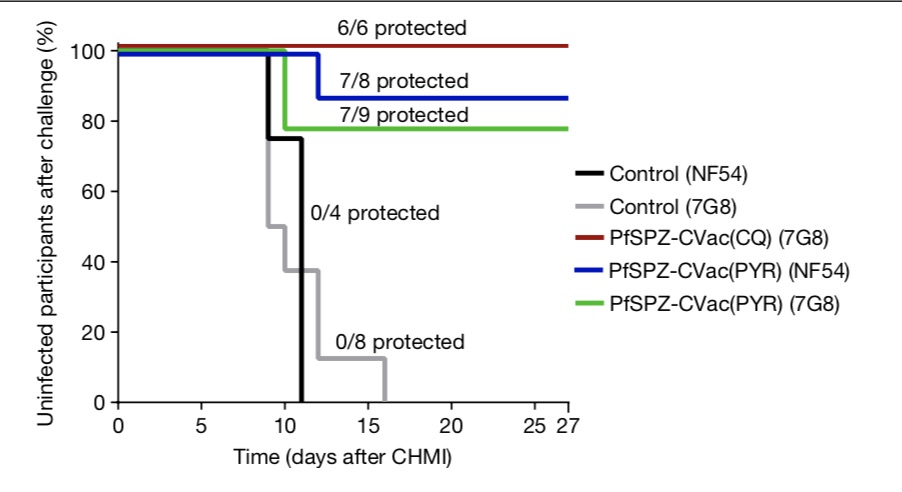 Minkah and others also mentioned that the development of a successful malaria vaccine A major obstacle is the large diversity of P. falciparum strains around the world.
Minkah and others also mentioned that the development of a successful malaria vaccine A major obstacle is the large diversity of P. falciparum strains around the world.
Minkah and others also commented that the reported vaccine still has several limitations that require attention. One of the most concerning is that this live parasite vaccine requires strict compliance with the regulations on taking concomitant drugs to prevent malaria caused by vaccination. This is feasible in controlled clinical trials, but if it is administered to billions of people Vaccines, it’s difficult to implement.
Another issue to consider is that any current pan-parasite vaccine strategy requires the production of sporozoites in live mosquitoes. There are huge challenges in expanding production.