In order to prevent the spread of new coronary pneumonia (COVID-19), China has adopted a large number of non-pharmaceutical interventions. As the epidemic in China gradually subsides, the situation in the United States, Spain, Italy and other countries is still grim. What kind of epidemic control policy should be chosen by governments and policy makers in various countries is actually a scientific question.
The latest study from the Chinese, American, and Italian teams pointed out that, as of now, regarding age, contact patterns, social distance, infection susceptibility, and the spread of COVID-19 The interaction between the dynamics is still unclear. They try to provide a scientific basis for more targeted long-term prevention and control strategies.
April 29th, local time, Fudan University School of Public Health, Italian ISI Foundation, Hunan Provincial Center for Disease Control, Italian Bruno Kessler Foundation, American State A research team from the Fogarty International Center of the National Institutes of Health (NIH) and the Biology and Social Technology System Simulation Laboratory of Northeastern University has published a study in the top academic journal “Science” “Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China “.
The study ’s corresponding authors are Professor Yu Hongjie of the School of Public Health of Fudan University, doctoral supervisor, director of the Key Laboratory of Public Health and Safety Education (Fudan University), and Bruno of Italy. Marco Ajelli, a computational epidemiologist at the Kessler Foundation.
The research team analyzed the contact investigation data of Wuhan and Shanghai before the outbreak of the New Crown Outbreak and during the outbreak, as well as from Hunan Provincial contact tracking information. The study found that during the implementation of the social distance alienation policy, the average daily contact between Wuhan and Shanghai decreased by about 80%, and most of the interaction was limited to families. The study also found that children aged 0-14 years are less susceptible to SARS-CoV-2 infection than adults aged 15-64 years, compared with people over 65 years old. Based on these data, the research team established a propagation model to study how the spread of the epidemic is affected by age differences and social distance. In addition, they predicted the impact of social distance and school closure on the spread of COVID-19. They believe that the implementation of the social distance policy during the outbreak in China is sufficient to control COVID-19. In addition, although the active closure of schools cannot stop the transmission itself, they can reduce the peak incidence by 40% -60% and delay the outbreak.
Overall, this study provides evidence that the interventions implemented in Wuhan and Shanghai, and the resulting changes in human behavior, have greatly reduced daily Engagement fundamentally reduces interaction. This has caused a sharp reduction in SARS-CoV-2 propagation.
The research team also proposed that designing a target strategy for long-term control of COVID-19 will be particularly important, including control strategies based on school and work, as well as large-scale detection and contact Person tracking. Future research should focus on perfecting age-specific assessments of infections, diseases, and infectiousness, which will help assess the impact of these strategies.
City mobility has declined during the epidemic, and home contact is the main social contact mode
City mobility has declined during the epidemic, and home contact is the main social contact mode
In order to assess the mixed age model associated with COVID-19 intervention Changes, the research team conducted contact investigations in two cities: the outbreak center Wuhan, and Shanghai, the largest and most densely populated city in southeastern China. During the outbreak, there were many imported cases and local transmission cases in Wuhan in Shanghai. The survey period is from February 1, 2020 to February 10, 2020, and the survey method is telephone survey.
Wuhan participants need to complete a questionnaire describing their contact behavior at two different times: First, December 24, 2019 to December 2019 A normal working day between 30 days, that is, before the Wuhan Municipal Health Commission officially announces the outbreak (used as a baseline); second, the day before the questionnaire survey, that is, during the outbreak. Participants in Shanghai are required to complete the same questionnaires used in Wuhan, but only need to report contacts during the outbreak.
In these phone surveys, “contact” is defined as two ways, one is face-to-face conversation, and the other is direct physical contact such as handshake.
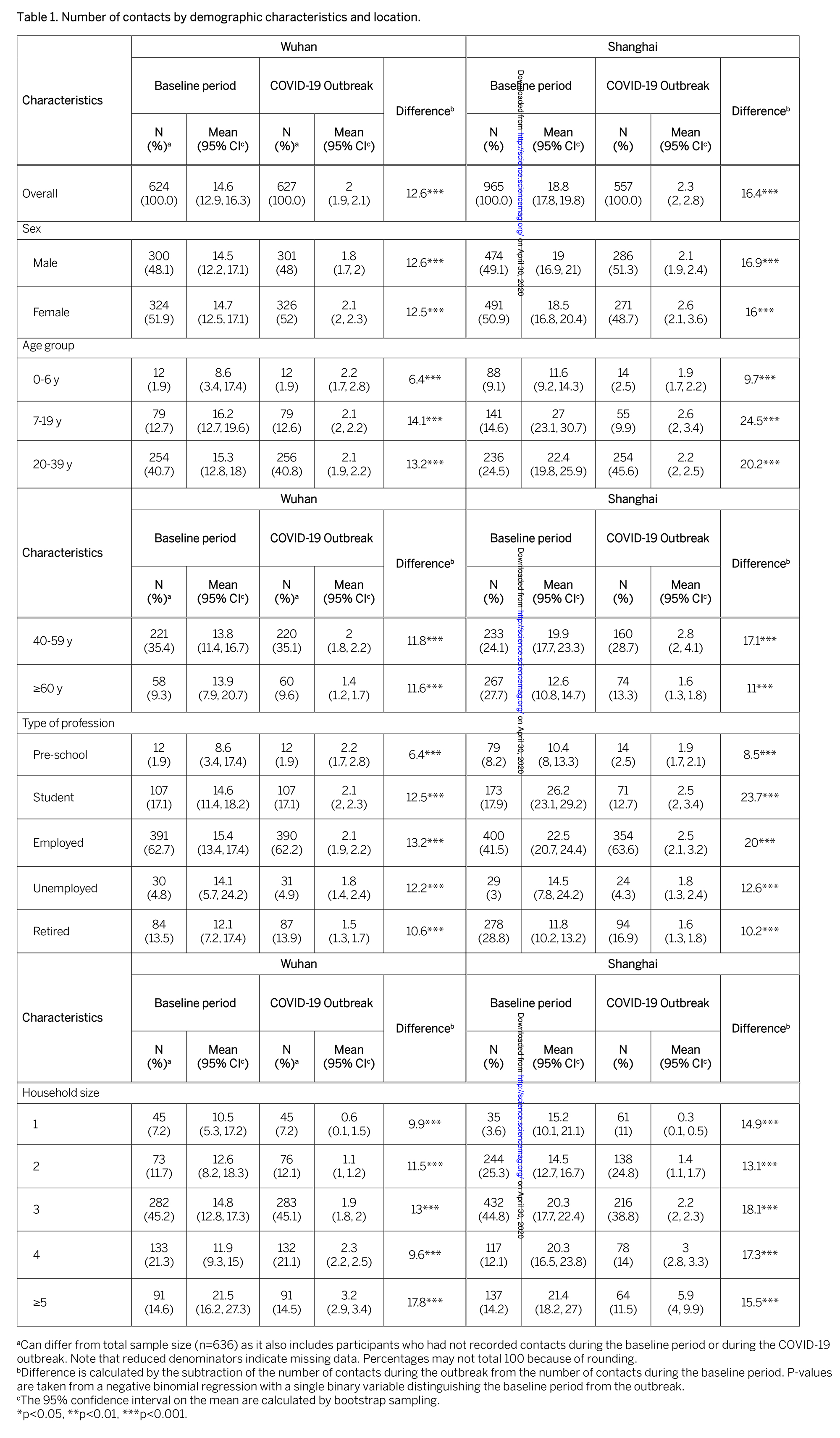
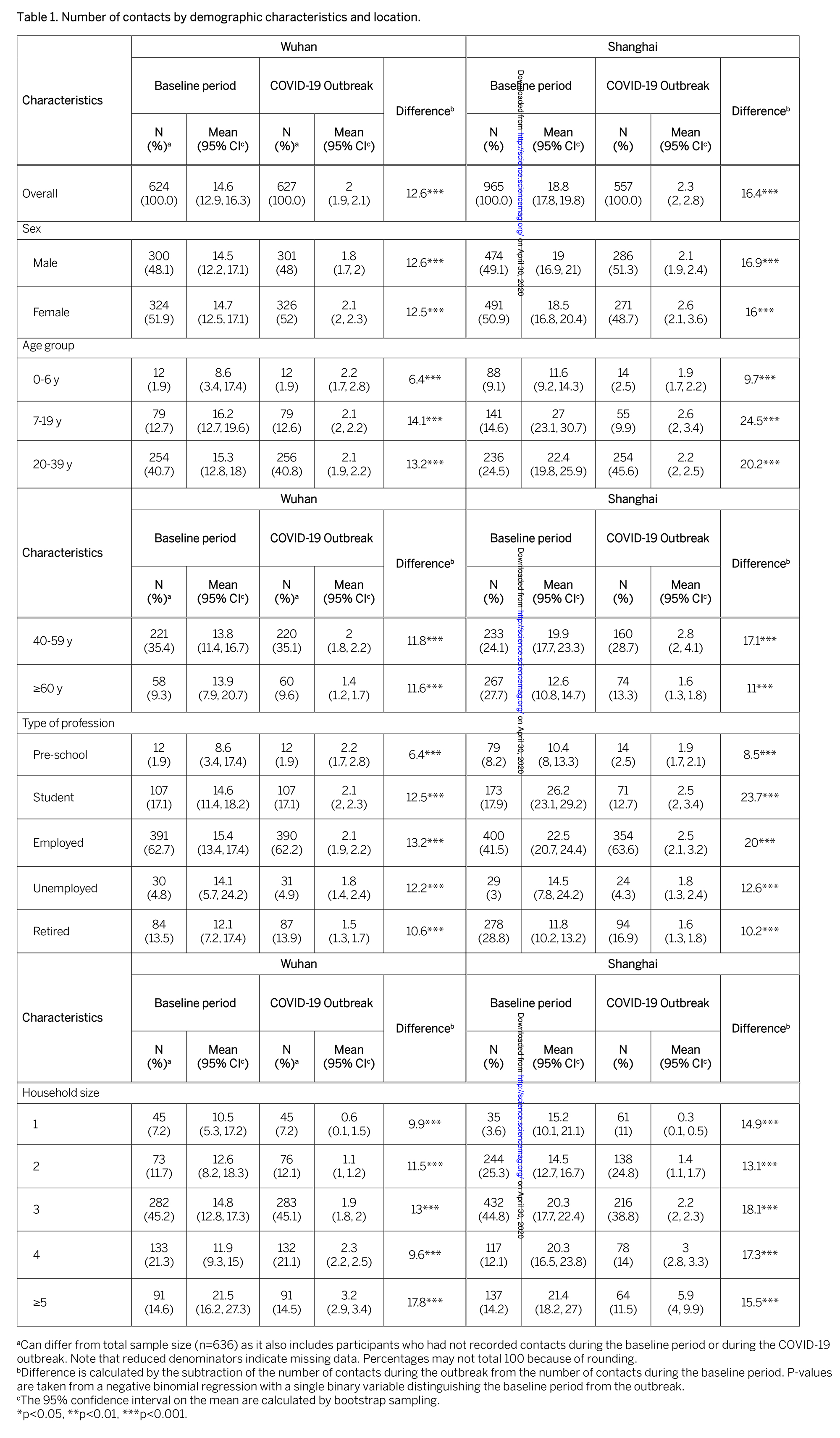
The study analyzed a total of 1,245 contacts reported by 636 participants in Wuhan and 557 participants reported by Shanghai 1296 contacts. In Wuhan, the average daily contact number of each participant decreased significantly, from 14.6 in the baseline period to 2.0 in the outbreak period. The decrease observed in Shanghai is even more pronounced, with the average number of daily contacts falling from 18.8 to 2.3.
 Baseline contact matrix for Wuhan (A) and Shanghai (D) (applicable to normal working days only). Each cell of the matrix represents the average number of contacts between individuals of a particular age group and other individuals, grouped by age. The color brightness indicates the number of contacts; the contact matrix during outbreaks in Wuhan (B) and Shanghai (E); the difference between the contact matrix during the baseline period in Wuhan (C) and (F) and that during the outbreak.
Baseline contact matrix for Wuhan (A) and Shanghai (D) (applicable to normal working days only). Each cell of the matrix represents the average number of contacts between individuals of a particular age group and other individuals, grouped by age. The color brightness indicates the number of contacts; the contact matrix during outbreaks in Wuhan (B) and Shanghai (E); the difference between the contact matrix during the baseline period in Wuhan (C) and (F) and that during the outbreak.
 Baseline contact matrix for Wuhan (A) and Shanghai (D) (applicable to normal working days only). Each cell of the matrix represents the average number of contacts between individuals of a particular age group and other individuals, grouped by age. The color brightness indicates the number of contacts; the contact matrix during outbreaks in Wuhan (B) and Shanghai (E); the difference between the contact matrix during the baseline period in Wuhan (C) and (F) and that during the outbreak.
Baseline contact matrix for Wuhan (A) and Shanghai (D) (applicable to normal working days only). Each cell of the matrix represents the average number of contacts between individuals of a particular age group and other individuals, grouped by age. The color brightness indicates the number of contacts; the contact matrix during outbreaks in Wuhan (B) and Shanghai (E); the difference between the contact matrix during the baseline period in Wuhan (C) and (F) and that during the outbreak.
While analyzing the baseline period, which is before the outbreak, the social contact patterns presented by Wuhan and Shanghai both show typical characteristics of mixed age contact. In contrast, during the outbreak of the epidemic, after implementing a strict social distance policy, most of the above features disappeared, leaving basically only contact within the family. In particular, according to the difference between the baseline and the outbreak matrix, it can be seen that the contact of the school-age group has completely disappeared.
Research believes that, in general, contact during the outbreak mainly occurs between family members (Wuhan 94.1%, Shanghai 78.5%). These findings are also in line with the trend of intra-city mobility data. Between early January and early February, urban mobility in Shanghai fell by 86.9% and Wuhan by 74.5%. Such a large decline in internal mobility and the majority of exposures occurring within the family during the epidemic result in aTo.
It is worth noting that when implementing strict social distance measures in Wuhan and Shanghai, workplace contact has not been completely eliminated, because some basic and important work still needs carry on.
Senior susceptibility increases with age: 0-14 year olds have the lowest risk of infection
Senior susceptibility increases with age: 0-14 year olds have the lowest risk of infection
Next, in order to understand social distance interventions and crowd contact The interaction between changes in patterns and the dynamics of the epidemic, the study also needs to consider potential age differences in infection susceptibility. The research team pointed out that this is currently a controversial topic, the reasons for which include little information about the age distribution of asymptomatic cases.
The research team analyzed the detailed epidemiological field investigation COVID-19 contact tracking information of Hunan Provincial Center for Disease Control and Prevention. In summary, all close contacts of reported COVID-19 cases in Hunan were subjected to 14-day medical observations using real-time RT-PCR. Those who tested positive were subsequently diagnosed with SARS-CoV-2 infection.
The research team conducted a generalized linear mixed model regression to illustrate the clustering and potential related structure of contacts who were exposed to the same index cases (such as within the family). They used the age group and sex of the contact person, the type of contact, and whether the contact person had traveled to Hubei / Wuhan as regression covariates.
They found that the susceptibility to SARS-CoV-2 infection increases with age. Individuals 0-14 years old have a lower risk of infection than individuals 15-64 years old [OR = 0.34 (95% CI: 0.24-0.49)]. In contrast, the risk of infection among the elderly aged 65 and above is higher than that of adults aged 15-64 [OR = 1.47 (95% CI: 1.12-1.92)].
The research team quoted the Shenzhen CDC, the Johns Hopkins University Bloomberg School of Public Health and other teams that published on the preprint platform medRxiv in March this year. A study further emphasized that there is still some controversy about susceptibility. Research by the Shenzhen Disease Control Center and other teams at the time believed that the susceptibility to the new coronavirus did not change with age.
If the epidemic is not controlled, the average incidence of infection after one year is 53% -92%
If the epidemic is not controlled, the average incidence of infection after one year is 53% -92%
The research team then discussed how their data provided a prevention and control strategy for COVID-19.
They point out that a key parameter that regulates epidemic dynamics is the basic infection number (R0). The so-called R0 refers to the average number of infections that an infected person transmits to other individuals without external intervention and no one has immunity. This study evaluated the impact of interventions on R0 and used next-generation matrix methods to quantify the changes in R0.
In addition, in order to illustrate the effect of mixed age contact modes on the outbreak dynamics, they developed a simple SARS-CoV-2 propagation model SIR. In the model, the population is divided into three epidemiological categories: susceptible, infected, and removed (people who recover or die). According to the estimation of the age-specific susceptibility to infection, susceptible individuals will be infected after contact with infected individuals, and the probability of occurrence of the contact is determined by the mixed mode estimate of each age group. The average time interval between two consecutive cases is 5.1 days.
 The impact of contact patterns on the spread of the epidemic, A, Wuhan; B Shanghai.
The impact of contact patterns on the spread of the epidemic, A, Wuhan; B Shanghai.
 The impact of contact patterns on the spread of the epidemic, A, Wuhan; B Shanghai.
The impact of contact patterns on the spread of the epidemic, A, Wuhan; B Shanghai.
In the early stage of the COVID-19 outbreak in Wuhan, that is, before the implementation of intervention measures, the R0 value was estimated to be 2.0-3.5. In this analysis, the research team extended the R0 range of the baseline period to 1-4. They found that considerable changes in contact patterns between Wuhan and Shanghai caused a sharp decrease in R0, and both Wuhan and Shanghai could fall below the epidemic threshold of 1. If it is assumed that there is no difference in the susceptibility of the population between different ages (Equal susceptibility), the conclusion is still similar.
 The incidence of infection one year after the first COVID-19 case, C, Wuhan; D Shanghai. span>
The incidence of infection one year after the first COVID-19 case, C, Wuhan; D Shanghai. span>
 The incidence of infection one year after the first COVID-19 case, C, Wuhan; D Shanghai. span>
The incidence of infection one year after the first COVID-19 case, C, Wuhan; D Shanghai. span>
Assuming the outbreak is not under control (no intervention measures, travel restrictions, or spontaneous group cooperation), that is, R0 range is 2-3, the study estimates that the outbreak is one After the year, the average infection rate is 53% -92%, and the difference between Wuhan and Shanghai is relatively small.
School closure is not enough to completely prevent the outbreak, and in the long run, the spread should be more targeted.
School closure is not enough to completely prevent the outbreak, and in the long run, the spread should be more targeted.
Next, the research team used the Model to estimate the impact of early large-scale school closures. Based on data from Shanghai, the study considered two different contact patterns: contact patterns during full holidays; contact patterns during normal working days, but removed contact at school.
The study also reminded that both of these situations are simplifications of school closure strategies. In fact, China closed schools in response to the COVID-19 pandemic, and all on-site education services were interrupted. However, contact patterns during school holidays indicate that some children still participate in additional educational activities, which is not uncommon.
 Limit the impact of school exposure on the spread of the epidemic.
Limit the impact of school exposure on the spread of the epidemic.
 Limit the impact of school exposure on the spread of the epidemic.
Limit the impact of school exposure on the spread of the epidemic.
The modeling of this study shows that the complete vacation contact mode can block the propagation of baseline R0 within 1.5 (Figure 3, A and C), The pattern of removing school contact on a normal working day can block the spread of baseline R0 within 1.2. For example, if the baseline R0 is 2.5, it is assumed that the average peak daily incidence rate will be reduced by 64% in the full holiday exposure mode. Under the model of removing school contact on normal working days, the average peak daily incidence rate was reduced by 42%.
The study believes that, in general, the school closure policy alone is not sufficient to completely prevent the outbreak of COVID-19, but it can affect the dynamics of epidemic transmission, thereby alleviating the hospital load. It should be emphasized that the population of 5-19 years old in Shanghai accounts for 9.5% of the total population, which is significantly lower than the average of all China (16.8%) and other countries (including Western countries); for example, the proportion of the United States is 19.7% .
The research team finally concluded that although the research still has many limitations, this modeling work can provide some insights into a nationwide prevention and control strategy for infection The possible impact of morbidity and peak morbidity.
They believe that perhaps the most important thing is that the implementation of a strict and rigid blockade strategy has great economic and psychological impact, “In the long run, more It is a better choice to block the transmission in a targeted manner. “